WELCOME TO HEAD & NECK ROBOTIC SURGERY IN THE H&N
Laryngeal cancer, most commonly squamous cell carcinoma, arises from the mucosal epithelium of the larynx and is frequently associated with risk factors such as tobacco use and alcohol consumption. It is anatomically classified into supraglottic, glottic, and subglottic tumors, each with distinct patterns of spread, lymphatic drainage, and prognostic implications. Glottic tumors often present early due to voice changes, whereas supraglottic lesions may remain asymptomatic until more advanced. Management depends on tumor staging and location and may involve transoral surgery, open partial laryngectomy, total laryngectomy, or non-surgical modalities such as radiation or chemoradiation. Organ preservation strategies (surgical and non-surgical) are prioritized where oncologically feasible, with careful consideration of functional outcomes related to voice and swallowing.
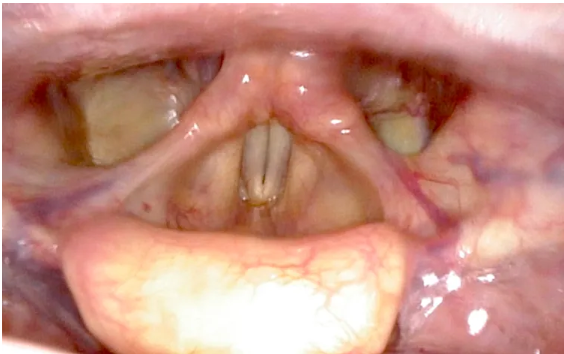
Adequate transoral exposure is a critical prerequisite for successful transoral surgery, particularly when targeting deep or distal structures such as the supraglottic larynx or hypopharynx. Achieving a clear, stable surgical corridor requires the use of specialized retractors.
Management of laryngeal cancer is typically coordinated through a multidisciplinary tumor board, which includes head and neck surgeons, radiation oncologists, medical oncologists, radiologists, pathologists, and other specialized staff. Each case is reviewed comprehensively, considering tumor site, stage, pathology, comorbidities, functional status, and patient preferences. The team determines the most appropriate evidence-based treatment plan, which may include surgery, radiotherapy, chemoradiation, or a combination. The goal is to ensure oncologic control while maximizing functional outcomes, such as voice preservation and swallowing.
TORS offers a minimally invasive approach for the resection of selected tumors in the supraglottic larynx and hypopharynx. Using the robotic system’s enhanced 3D visualization, tremor-free motion, and articulated instruments, surgeons can perform precise resections with en bloc removal with adequate oncologic margins. Benefits of the minimally invasive approach include reduced morbidity, shorter hospital stays, improved swallowing outcomes, and the potential to avoid tracheostomy or more extensive open procedures.
Patient safety is a transversal priority throughout the entire treatment process, guiding every clinical decision. The selection of candidates for TORS is based on a rigorous evidence-based approach, integrating tumor characteristics, imaging findings, and anatomical accessibility with current best practices and clinical guidelines. Not all patients are suitable for TORS. Treatment must be personalized, aligning oncologic goals with the patient’s overall health, functional status, and individual values and preferences. This is a patient-centered decision-making process. Ultimately, surgical expertise, institutional experience, and careful preoperative assessment are key to maximizing outcomes and minimizing risks.

Related posts: